Could it be KC (KERATOCONUS)?
KC File #5: Sleuthing out the Source of Monocular Vision Loss
Tracy “Tracker” Swartz, OD, MS, FAAO, Huntsville, AL

A 24-year-old female was referred to me for a dry eye evaluation. The referring optometrist had recorded changing refractions in her right eye across several visits. More concerningly, the formerly 20/20 right eye was now only correctible to 20/30 or 20/50, while the left eye had been stable and 20/20 all along. This patient had a history of Bell’s palsy at age 10 so the referring doctor, not unreasonably, suspected dry eye related to lid closure issues on the affected right side. She was prescribed a topical immunomodulator for twice-daily use for 6 weeks, but the treatment did not improve her vision.
 Further review of her refractive history showed that not only had the refraction changed frequently, but the cylinder component had increased by 1.00 D and the axis of astigmatism in the right eye was highly variable (66°, 136°, and 100° at different visits), which we don’t expect to see with a normal progression of refractive error. At her last two exams, there was a mismatch between the manifest and autorefractions obtained the same day—something that is common in keratoconus due to irregular astigmatism.
Further review of her refractive history showed that not only had the refraction changed frequently, but the cylinder component had increased by 1.00 D and the axis of astigmatism in the right eye was highly variable (66°, 136°, and 100° at different visits), which we don’t expect to see with a normal progression of refractive error. At her last two exams, there was a mismatch between the manifest and autorefractions obtained the same day—something that is common in keratoconus due to irregular astigmatism.
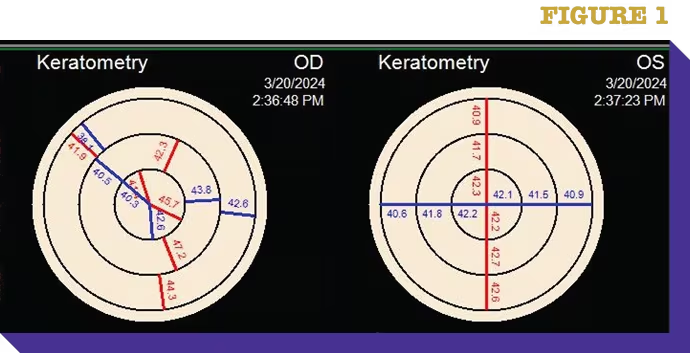
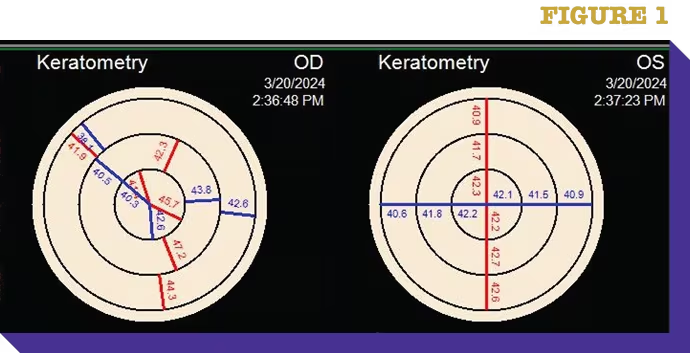
Topography showed significant inferior nasal steepening in the right eye. Dry eye can also cause inferior steepening, but in that case, we typically see an improvement with treatment—one of the reasons I like being able to perform topography for my dry eye patients as well as keratoconus suspects. The topography also showed skewing of the keratometry in the right eye compared to the left eye (Fig. 1). The inferior-to-superior (I-S) difference in the outer ring (41.9 D superiorly vs. 44.3 D inferiorly) and the relatively steep 45.7 central reading in the right eye were highly suspect for keratoconus, too.
I diagnosed this patient with progressive keratoconus (not dry eye disease) in the right eye and she underwent iLink cross-linking in April, 2024. Six months later, her cornea had stabilized, allowing her to remain in spectacles with good quality vision. Keratoconus often presents asymmetrically, as it did in this case, but we know it is a bilateral disease, so I will continue to watch her left eye closely every 3-4 months. Any of the most commonly required progression criteria
 for cross-linking would trigger a referral back to the iLink
surgeon: An increase of ≥1.00 D in steepest keratometry; an
increase of ≥1.00 D of cylinder in subjective or manifest
refraction; or a myopic shift of ≥0.50 D of spherical equivalent
refractive error (MRSE).
for cross-linking would trigger a referral back to the iLink
surgeon: An increase of ≥1.00 D in steepest keratometry; an
increase of ≥1.00 D of cylinder in subjective or manifest
refraction; or a myopic shift of ≥0.50 D of spherical equivalent
refractive error (MRSE).
For this patient, refractive changes preceded loss of acuity, and
we were fortunate to catch her just as she was starting to lose
lines of vision.
By following the KC clues that are hiding in plain sight, you can help your patients get diagnosed and treated earlier, preserving their vision and corneal stability.